EVO ICL may be best-kept secret in refractive surgery
As demand for this lens grows, the need for expert refractive comanagement will expand as well.

Every day, patients express interest in spectacle independence. They often think laser in situ keratomileusis (LASIK) is the only way to accomplish this because it is the refractive procedure with which they are most familiar. I always use these inquiries as an opportunity to explain that there are a variety of excellent interventions that can be employed to achieve reduced or total spectacle independence, and the EVO Visian (STAAR) ICL (implantable Collamer lens) is one of them.
Although the EVO ICL gained FDA approval in the United States just this year, it has a long and successful history outside the country, where more than 2 million have been implanted during the past 15 years.
Our practice, Parkhurst NuVision LASIK Eye Surgery in San Antonio, Texas, was the highest-volume EVO provider involved in the FDA clinical trial (NCT04283149) responsible for its US approval, and we are one of the first practices in the country to offer EVO to our patients.
After hearing about the FDA approval, patients have flown in from Massachusetts, New York, Idaho, Nevada, California, Florida, Minnesota, and Michigan to have ICL surgery here. As demand for these refractive lenses grows, the need for expert optometric comanagement—from patient selection to preoperative and postoperative care—will expand accordingly.
Benefits
Historically, ICLs have been the surgical solution for high myopes with or without astigmatism, as well as those with thin corneas, irregular corneas, or those who would have an insufficient residual stromal bed after laser vision correction. Because of this, ICLs are often positioned as an excellent option for patients who do not qualify for LASIK; however, they are not only for those patients.
The EVO lens can correct vision for a wide range of eye prescriptions—from 3 to 20 diopters (D) of myopia and 1 to 4 D of astigmatism. Due to its ability to correct large amounts of myopia and astigmatism, it has often been shown to produce postoperative vision that is better than preoperative vision.1 In the FDA clinical trial, the average EVO postoperative vision was better than 20/20.
What’s more, in the toric ICL study (NCT04516772), approximately 75% of patients gained at least 1 line of vision.2 Myopes and myopic astigmats have better vision if the correction is closer to the nodal point (less minification). Anecdotally, we have had numerous patients who were once given diagnoses of amblyopia (20/30) but who after ICL are 20/20.
One important advantage associated with the EVO is that this ICL can be used in patients with dry eye. As a result, it is the procedure of choice when we are dealing with patients seeking a surgical solution because of contact lens–induced dry eye disease (DED) or contact lens–associated DED.
Studies suggest that there is a lower risk of DED in ICL patients compared with laser vision correction patients, and this has been validated anecdotally in our practice.3 One study looked at the tear film osmolarity in individuals 10 years after having ICL surgery and compared it to virgin eyes and found no difference.4
Although the EVO lens is designed to provide permanent vision correction, it is removable and replaceable. Unlike laser-based refractive procedures, it is additive and does not require corneal tissue excision.
What’s new with EVO?
The EVO lens is produced from Collamer, a proprietary 2-hydroxyethyl methacrylate/porcine collagen–based biocompatible polymer material and a UV-absorbing chromophore. EVO stands for “evolution,” and this refers to the fact that the EVO lens is a newer iteration of an earlier version of the Visian ICL.
Figure 1.The EVO ICL 360-µm central port allows sufficient aqueous flow from the posterior chamber to the anterior chamber.
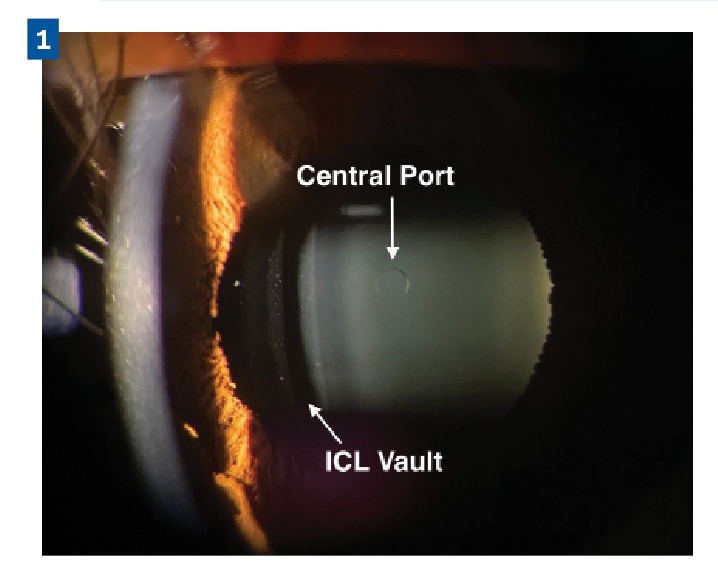
The biggest difference between EVO and the original Visian ICL is that the new lens is designed with a central hole. The 360-µm central port allows sufficient aqueous flow from the posterior chamber to the anterior chamber, which maintains the normal physiology of the anterior segment of the eye and eliminates the need for a preoperative iridotomy (PI) (Figure 1). This change streamlines the preoperative process because performing the PI used to require a separate preoperative appointment, which was inefficient. The port does not significantly alter the optical performance of the EVO lens compared to conventional ICLs, with studies demonstrating equivalent optical quality variables.5
Patient selection
ICLs are for patients with myopia (–3 to –20 D) and myopic astigmatism (1 to 4 D). As with all refractive procedures, careful patient selection is critical to ensuring postoperative satisfaction.
When evaluating a patient, we want to make sure they discontinued soft contact lens wear and their refraction is stable. We consider refractive stability as less than 0.5 D of change within the past 6 to 12 months.
We also want to make sure the patient has open angles and a healthy endothelium. Poor candidates are those who have narrow angles or any endothelial disease.
When a patient comes in for a consultation, we take a corneal tomography scan to get views of the anterior chamber depth (ACD). We get precise measurements of the central cornea and make sure they do not have any corneal opacities or significant corneal pathology, such as keratoconus. We also check the retina, to be sure there are no retinal tears; if there are, we get those treated prior to ICL surgery.
Because of the high levels of myopia, it can help to do a contact lens over-refraction, to account for vertex. The 2 most important measurements necessary to qualify a patient for ICL surgery are manifest refraction and ACD.
The FDA study required an ACD 3 mm or greater from posterior surface of the cornea to the anterior surface of the crystalline lens. Outside the United States, one study showed great results from ICL surgery in eyes less than 3 mm, with 1 eye having an ACD of 2.3 mm.6
Preoperative and postoperative care
To be able to order the EVO ICL, we need to know the size and power of the lens. We use high-frequency ultrasound to size the ICL. Sizing of the ICL affects the vault; therefore, precision is essential.
Although the EVO central hole reduces the likelihood of cataract formation, it is still important to make sure you have enough vault—especially in the case of toric ICLs. If the vault is too small, the lens can rotate.
After we have detailed intraocular measurements, a free online ICL sizing calculator (www.iclsizing.com) can predict the vault for each ICL size through the use of a dedicated nomogram. The nomogram considers the inner ciliary body diameter, as well as the lens rise, the scotopic pupil size, and the lens power.
In our practice, the surgery takes 5 to 7 minutes and both eyes are done on the same day. We see the ICL patients 1 day, 1 week, and 1 month after surgery, and at these appointments we check intraocular pressure (IOP) and vault.
Figure 2. The vault over the EVO ICL should be approximately 250 to 750 µm over the natural crystalline lens.
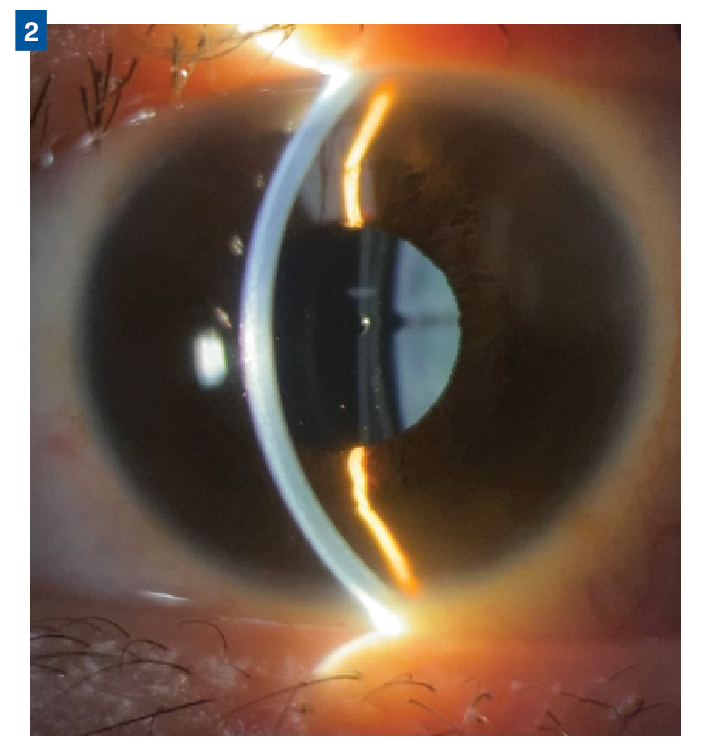
The average postoperative visual acuity among ICL patients at our practice is between 20/15 and 20/25. If eye pressure is elevated 1 day postoperatively, it is most likely because of remaining viscoelastic. It is important to document the vault. The size of the vault should be approximately 250 to 750 µm (Figure 2).
The EVO is implanted within the posterior chamber of the eye, directly behind the iris and in front of the natural crystalline lens. Because the central port allows for improved circulation of aqueous around the natural lens, it has reduced the incidence of postoperative IOP spikes and pupillary block. This design is also associated with less visually significant anterior subcapsular cataract formation compared with earlier ICL models; this also is due to the efficient fluid dynamics around the anterior lens capsule.7
Patient satisfaction
A STAAR survey of more than 1500 EVO ICL patients found that 99.4% said they would undergo the procedure again.8 Many of these patients who opt for EVO ICLs in our practice previously had dryness associated with contact lenses, and now they do not have the hassle of contacts or dry eye. They wake up in the morning and can see unaided. These patients are among the happiest refractive surgery patients we have treated.
When patients express interest in spectacle independence, we have a responsibility to counsel them about all available interventions. To do that, we must be as knowledgeable about the newest options as we are about those with the longest track record. By keeping up with the latest refractive surgery procedures and proactively discussing them, we are doing our best for our patients while making the most of our practice.
References
1. Kamiya K, Shimizu K, Igarashi A, Komatsu M. Comparison of Collamer toric implantable [corrected] contact lens implantation and wavefront-guided laser in situ keratomileusis for high myopic astigmatism. J Cataract Refract Surg. 2008;34(10):1687-1693. doi:10.1016/j.jcrs.2008.06.030
2. STAAR Visian Toric ICL post-approval study (TICL-PAS). ClinicalTrials.gov. Updated October 26, 2022. Accessed August 11, Dec. 14, 2022. https://clinicaltrials.gov/ct2/show/NCT04516772
3. Ganesh S, Brar S, Pawar A. Matched population comparison of visual outcomes and patient satisfaction between 3 modalities for the correction of low to moderate myopic astigmatism. Clin Ophthalmol. 2017;11:1253-1263. doi:10.2147/OPTH.S127101
4. Gjerdrum B, Gundersen KG, Lundmark PO, Potvin R, Aakre BM. Prevalence of signs and symptoms of dry eye disease 5 to 15 after refractive surgery. Clin Ophthalmol. 2020;14:269-279. doi:10.2147/OPTH.S236749
5. Kamiya K, Shimizu K, Saito A, Igarashi A, Kobashi H. Comparison of optical quality and intraocular scattering after posterior chamber phakic intraocular lens with and without a central hole (hole ICL and conventional ICL) implantation using the double-pass instrument. PLoS One. 2013;8(6):e66846. doi:10.1371/journal.pone.0066846
6. Kamiya K, Shimizu K, Igarashi A, et al. Posterior chamber phakic intraocular lens implantation in eyes with an anterior chamber depth of less than 3 mm: a multicenter study. Sci Rep. 2018;8(1):13322. doi:10.1038/s41598-018-31782-y
7. Packer M. The implantable collamer lens with a central port: review of the literature. Clin Ophthalmol. 2018;12:2427-2438. doi:10.2147/OPTH.S188785
8. Patient survey, STAAR Surgical ICL Data Registry, 2018.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.