Surprising findings from the DRCR Retina Network Protocol AA
These results emphasize the importance of evaluating the midperipheral and peripheral retina in diabetes in addition to the posterior pole and performing ultra-widefield fluorescein angiography for not only accurate diabetic retinopathy staging, but also for likelihood of significant progression based on disease severity and predominantly peripheral lesions.

Recently published and anticipated results from the Diabetic Retinopathy Clinical Research Retina Network (DRCR.net) Protocol AA yielded the surprising finding that predominantly peripheral lesions (PPL) using ultra-widefield (UWF) color retinal imaging were not predictive of significant, 2-step worsening on the Diabetic Retinopathy Severity Scale (DRSS)1, contrary to previous findings from several single-center studies.2,3
The initial study, conducted by investigators at the Joslin Diabetes Center in Boston, Massachusetts, found that PPL were highly and significantly associated with 2-step worsening (3.2× risk) and proliferative DR (PDR; 4.7× risk) over 4 years.2
An example of 2-step worsening would be moderate nonproliferative DR (NPDR) worsening to severe NPDR. In Protocol AA, however, primary analysis over 4 years of follow-up showed no significant association between color PPL and 2-step worsening. Similarly, secondary analysis found no association between color PPL and progression to PDR.
PPL demonstrated on ultra-widefield fundus fluorescein angiography (UWF-FA) were significantly associated with increased risk of both outcomes in Protocol AA, independent of baseline DRSS, although less so than reported by Silva et al in their 2015 paper (HR for 2-step worsening with UWF-FA PPL, 1.72; P < .001). The Protocol AA authors conclude that FA-PPL but not color-image PPL have predictive value for NPDR progression and should be included in future DR studies (with the caveat of increased time, cost, and adverse events with inclusion of FA).
Many optometrists and ophthalmologists have turned to UWF for identification and grading of DR severity, as well as for determining surveillance intervals based on not only DR severity but also the presence or absence of PPL seen on color UWF imaging. Silva et al found that eyes with color PPL were nearly 5 times more likely to develop PDR during the succeeding 4 years, whereas Protocol AA found that eyes with color PPL were less likely to develop PDR during the same interval (not statistically significant), a big disparity. What are those of us in primary eye care—even retinal specialty practices—to make of this discrepancy?
Protocol AA is a multicenter study of more patients and eyes from a more diverse study population than was the case in the Joslin Study (566 vs 103 study eyes; more women and members of ethnic minority populations). DRSS grading was also more precise in Protocol AA with a distinction between Level 43 (moderate NPDR) and Level 47 (moderately severe NPDR), whereas the single-center Joslin study lumped these 2 stages together as “moderate NPDR.”
The authors note that follow-up was somewhat attenuated due to the COVID-19 pandemic, and that identification of color PPL may have been hindered by insufficient visualization of the superior and inferior retina with use of only one of the available UWF imaging systems (SLO produced images with the P200Tx; Optos California).
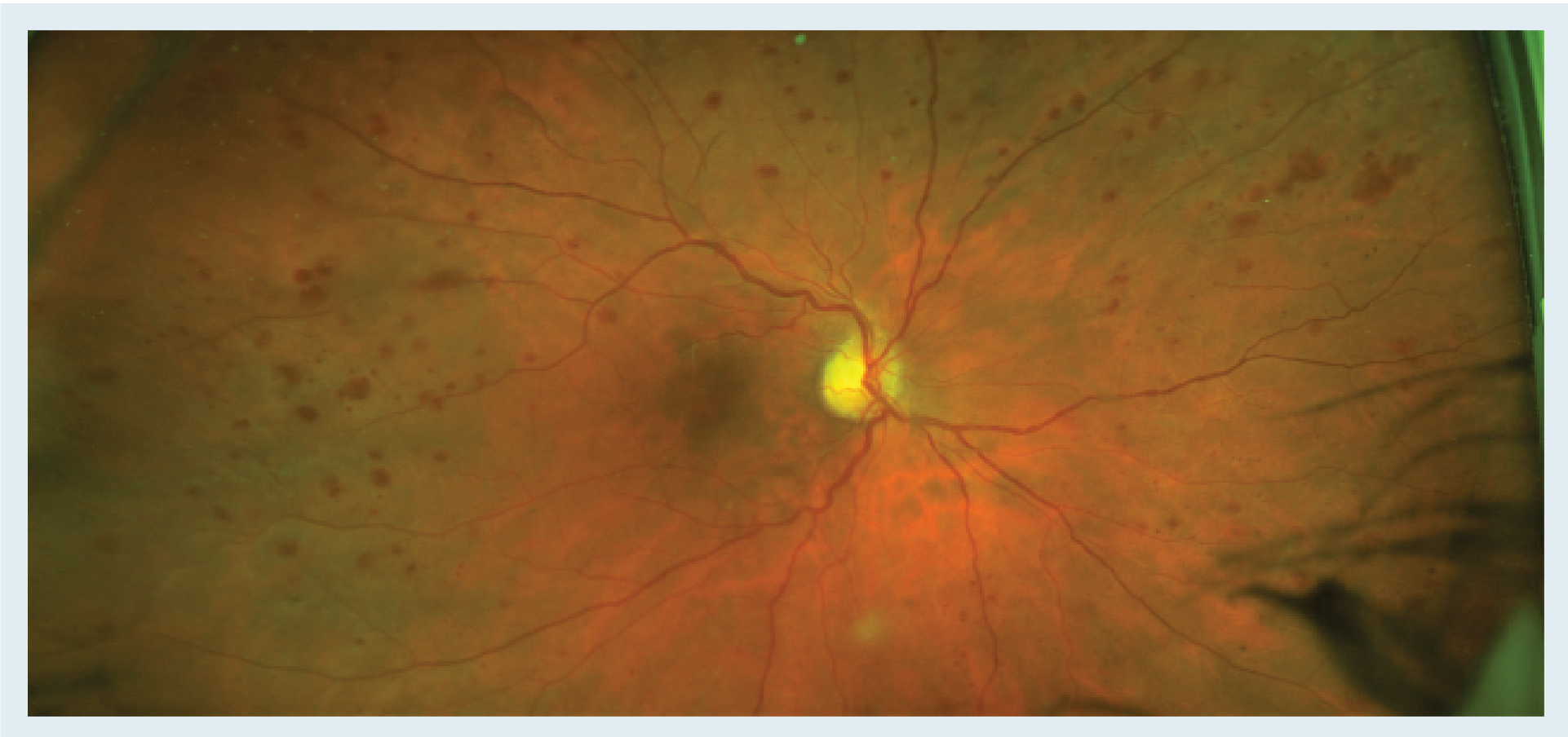
Figure. Here is an example of a patient with predominantly peripheral lesions using ultra-widefield color retinal imaging. Although DRCR.net Protocol AA found that this does not predict significant progression over 4 years, the abundance of peripheral lesions seen here compared to those seen in the posterior pole supports a diagnosis of severe nonproliferative diabetic retinopathy, as well as closer monitoring and/or referral to a retinal specialist and consideration for anti-VEGF therapy. (Image courtesy of A. Paul Chous, OD, MA, FAAO)
Another recent study has shown that mydriasis and manual lid elevation significantly improved visible retinal area (VRA) with the Optos system4 and it remains possible that true-color imaging systems would have revealed color PPL lesions more consistent with those seen by FA PPL.5
However, UWF imaging allows observation of roughly 50% more retinal area than does standardized, 7-field photography (SSFP) as has been used in virtually all DR studies since the Early Treatment Diabetic Retinopathy Study (ETDRS), and even more compared with single-image, 45°, color retinal photography commonly used in clinical practice during the last 25 years.
We would expect UWF to reveal more lesions consistent with DR based on increased VRA. Both the Joslin Study and Protocol AA found that use of color UWF imaging not only revealed more DR lesions but, more importantly, increased graded DR severity in 10% and 12.5% of eyes, respectively, compared with SSFP.
More accurate grading of DR severity is of utmost importance because it directly affects patient follow-up, prognosis, and treatment decisions. If a patient has severe NPDR rather than moderate NPDR based on significant peripheral retinal lesions identified by UWF, but not seen with examination of the posterior pole in isolation, the surveillance interval should be significantly shortened and treatment with anti-VEGF therapy becomes an important option for that patient based on correct staging of disease severity.6 This VRA benefit obviously applies to detection of any peripheral retinal pathology, as any user of UWF imaging will attest—a fact that must be remembered even if color PPL is not useful for predicting progression of NPDR in and of itself.
In sum, these new findings from DRCR.net underscore the importance of evaluating the midperipheral and peripheral retina in diabetes in addition to the posterior pole, as well as additional benefit of performing UWF-FA for not only accurate DR staging but also likelihood of significant progression based on disease severity and PPL. Figure depicts a patient found to have PPL with UWF color imaging.
References
1. Marcus DM, Silva PS, Liu D, et al; DRCR Retina Network. Association of predominantly peripheral lesions on ultra-widefield imaging and the risk of diabetic retinopathy worsening over time. JAMA Ophthalmol. 2022;140(10):946-954. Published correction in JAMA Ophthalmol. Published online November 17, 2022.
2. Silva PS, Cavallerano JD, Haddad NMN, et al. Peripheral lesions identified on ultrawide field imaging predict increased risk of diabetic retinopathy progression over 4 years. Ophthalmology. 2015;122(5):949-956. doi:10.1016/j.ophtha.2015.01.008
3. Elmasry MA, Silva PS, Cavallerano J, Pisig AU, Aldairy Y, Sun JK, Aiello LP. Incorporating predominantly peripheral diabetic retinopathy (DR) lesion identification in a teleophthalmology program predicts DR progression over 4 years in eyes with early DR. Investig Ophthalmol Vis Sci. 2018;59(9):740.
4. Jacoba CMP, Ashraf M, Cavallerano JD, et al. Association of maximizing visible retinal area by manual eyelid lifting with grading of diabetic retinopathy severity and detection of predominantly peripheral lesions when using ultra-widefield imaging. JAMA Ophthalmol. 2022;140(4):421-425. doi:10.1001/jamaophthalmol.2021.6363
5. Rajalakshmi R, Prathiba V, Arulmalar S, Usha M. Review of retinal cameras for global coverage of diabetic retinopathy screening. Eye (Lond). 2021;35(1):162-172. doi:10.1038/s41433-020-01262-7
6. Brown DM, Wykoff CC, Boyer D, et al. Evaluation of intravitreal aflibercept for the treatment of severe nonproliferative diabetic retinopathy: results from the PANORAMA randomized clinical trial. JAMA Ophthalmol. 2021;139(9):946-955. doi:10.1001/jamaophthalmol.2021.2809
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.