Know the many facets of diabetic retinopathy
One of the challenges of managing diabetic retinopathy is the numerous intricacies and nuances in its presentation outside of “classic textbook.”
Case report
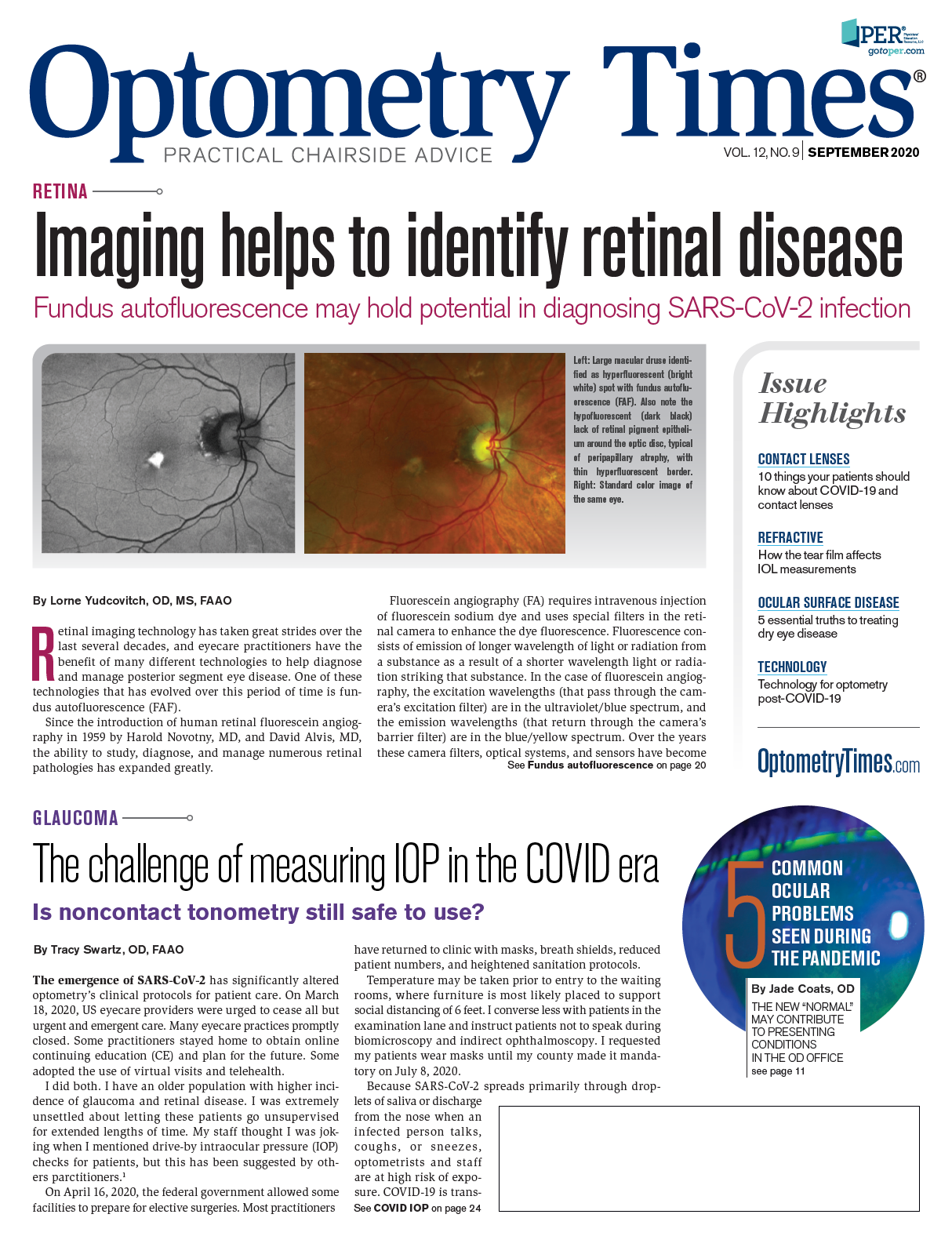
A 52-year-old African-American male with type 1 diabetes had been referred 5 years earlier for proliferative diabetic retinopathy (PDR, Figure 1) and had undergone treatment, including multiple intravitreal anti-VEFG (vascular endothelial growth factor) injections in both eyes and panretinal photocoagulation initially in both eyes (Figure 2). Those procedures were followed by pars plana vitrectomy (PPV) in the right eye as the result of progression of tractional retinal detachment involving his macula (Figure 3).
He did not have direct vitreomacular traction in the left eye as he was demonstrating a progressive increase in his central foveal thickness and enlarging intraretinal cystic spaces (Figure 4) while reporting progressive loss of his vision. These findings were initially thought to be the result of diabetic macular leakage, but they were not responding to conventional anti-VEGF injections.
A fluorescein angiography (FA) was performed to identify the source of this possible leakage. Although the FA showed leakage of active neovascularization elsewhere (NVE) and diffuse macular leakage in the right eye, there was no macular leakage in the left eye and mild leakage of an old patch of neovascularization of the disc (NVD, Figure 5). This was contrary to the optical coherence tomography (OCT) findings that were showing the presence of epimacular (also called epiretinal) membrane (EMM) in the right eye and the cystic spaced left eye (Figure 6).
An alternative wide-field OCT was performed to assess the vitreoretinal interface and the retinal thickness beyond the conventional central 30Ë scan. The results were remarkable, showing that tractional forces and tractional retinal detachment (TRD) extending from the disc toward the nasal retina was responsible for the macular appearance (Figure 7). This pulling force is similar to dragging a rope tangentially to raise a sail.
The patient underwent PPV and repair of the TRD. Following this procedure, the resolution of traction resulted in significant reduction of the schisis cavities in extramacular retina (Figure 8). Macular schisis, although improved, will take several months to slowly subside.
Discussion
It is easy for clinicians to become accustomed to the routine and become complacent in practice methods. However, when unconventional and unexpected presentations arrive, clinicians need to step outside of the box and think of alternatives that help in managing patients and improving their quality of life. Eyecare practitioners have incredible technology such as ultra widefield fundus imaging and spectral domain OCT at their disposal; however, they don’t always use them to their maximum capabilities.
Related: Patient perception of good vision a trap leading to loss
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.