When cataract outcomes are confounded by dry eye
Three cases illustrate the perils of failing to address ocular surface disease
We all want our patients to have a great experience when it is time for cataract surgery. A lot of thought, patient education, and counseling goes into the preoperative process to ensure that results can meet or exceed patient expectations.
But undiagnosed ocular surface disease can foil the best-laid plans. According to the Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study, nearly 80 percent of patients coming in for cataract surgery have signs of at least stage 2 dry eye or worse, although most didn’t have a dry eye diagnosis prior to the study.1 Several recent studies have also shown that meibomian gland dysfunction (MGD) is present in 50 to 60 percent of the cataract surgery population.2,3
Dry eye and MGD can affect preoperative IOL measurements as well as patients’ comfort, speed of recovery, and postoperative satisfaction. Here are three case studies that illustrate why ODs can’t afford to ignore MGD in cataract surgery patients.
Case 1
Six years ago, I saw a 55-year-old female patient who had undergone bilateral implantation of multifocal intraocular lenses (IOL) at our center about 1 year prior. A former -10.00 D myope, she was initially thrilled with her 20/20 OD and 20/40 OS refractive outcome.
However, over the course of a year, her distance vision had declined to 20/30 OD and 20/50 OS. Although the patient had some symptoms of dry eye, she thought those were normal and wasn’t too bothered by them. Her chief complaint was fluctuating vision, especially when working at the computer, where she spent a lot of time.
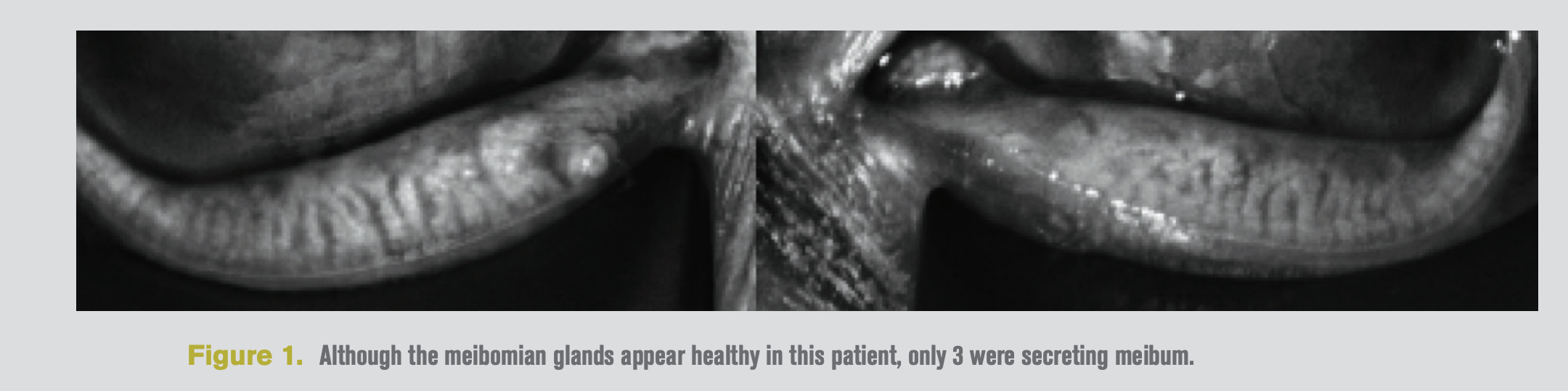
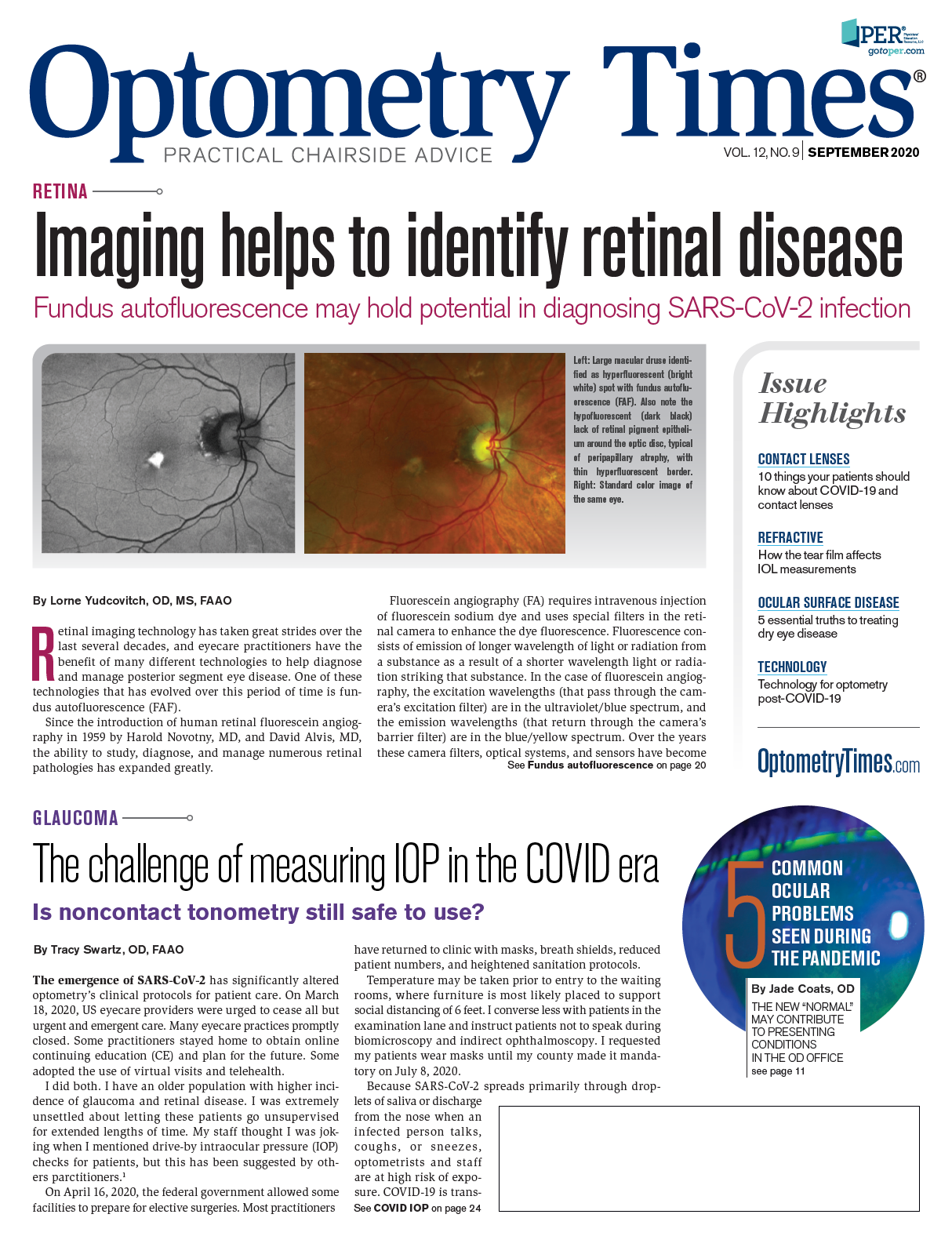
In examining the meibomian glands, I found very little atrophy (Figure 1), but the glands were obstructed; only three were secreting meibum.
We treated her with LipiFlow thermal pulsation therapy (Johnson & Johnson Vision). After treatment, her vision improved to 20/20 OD and 20/30 OS, which was even better than it had been initially after cataract surgery.
We continue to manage her dry eye and MGD with daily cyclosporine and fish oil supplements, and thermal pulsation therapy every 2 to 3 years. With this regimen, she has improved comfort and more stable vision, rather than the fluctuations she found so bothersome in the past. While this patient uses hot compresses occasionally at home, it is important to note that compresses alone will not clear obstructed glands—they can help only to extend the duration of effect after the obstructed meibum has been evacuated.
The lower activator price in the last several years makes it easier for patients to afford repeat thermal pulsation treatments for better maintenance of their meibomian glands. Our office also bundles the price in with premium IOL surgery (when thermal pulsation is recommended) to give the patient a bigger discount and greater incentive to have thermal pulsation in advance. With this approach, we have an acceptance rate of about 60 percent for preop LipiFlow procedures.
Case 2
An 81-year-old gentleman underwent cataract surgery on his right eye in December 2019. His optometrist had treated him for mild dry eye in the past, and at the preoperative appointment he reported only mild symptoms. Best-corrected acuity in the operative eye was 20/30 due to cataract. The patient wanted to reduce his dependence on glasses and get the latest IOL that would offer the possibility of good vison at all distances.
He had a Panoptix (Alcon) trifocal IOL implanted in the right eye. Surgery was uneventful. By 2 weeks postop, his distance acuity was 20/60 uncorrected, 20/40 with correction, and the patient was absolutely miserable with both his poor vision and the discomfort he was experiencing.
He said the right eye felt so dry and irritated he could hardly open it. Objectively, the cornea looked good, with minimal staining, but the patient was highly symptomatic. We prescribed Cequa (cyclosporine 1%, Sun Pharmaceuticals), warm compresses, and frequent lubrication with preservative-free artificial tears.
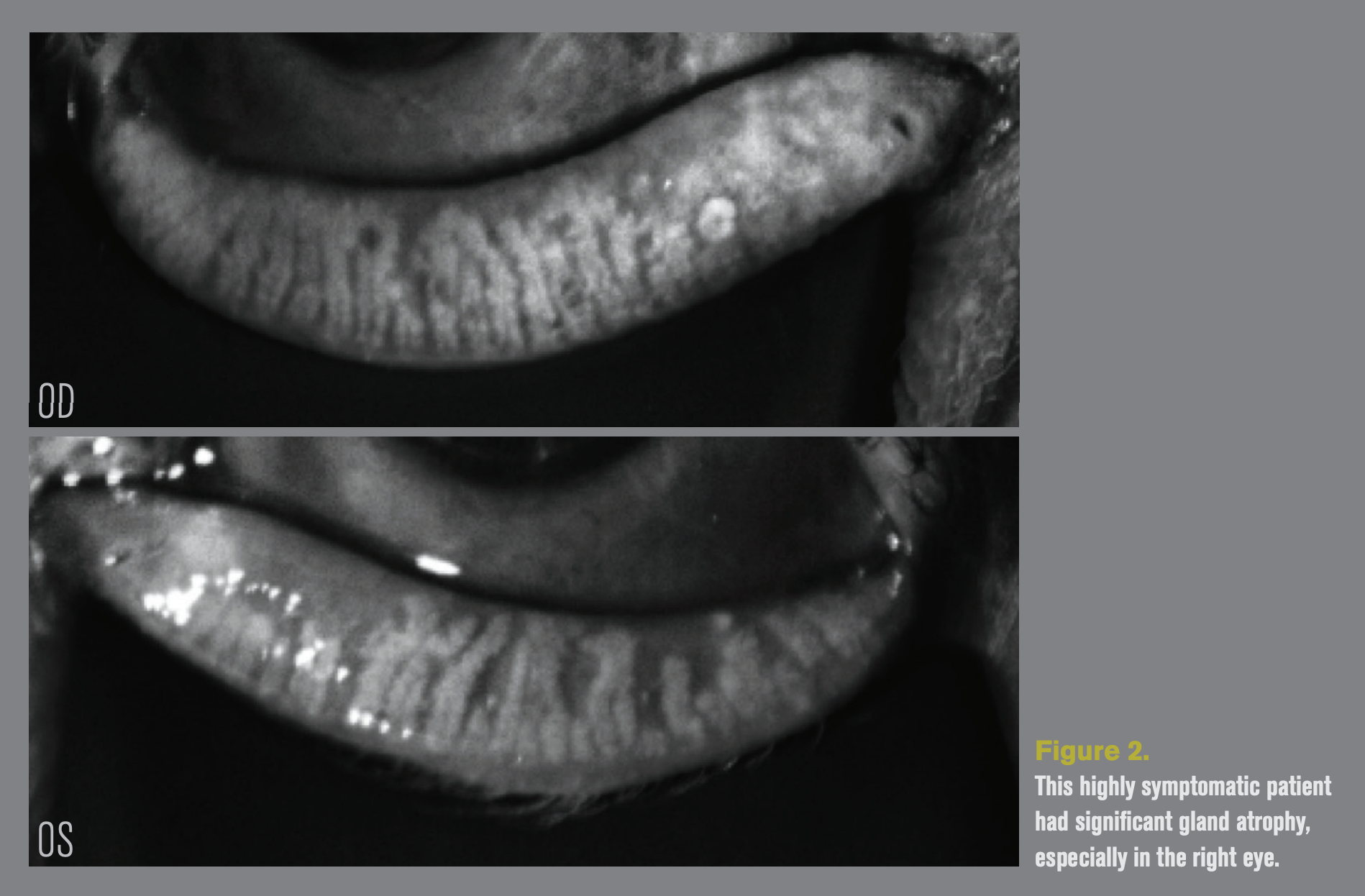
Meibography showed that he had severe meibomian gland atrophy, with about 45 percent gland loss in the left eye and 30 percent in the right eye (Figure 2). To improve his satisfaction with the premium IOL surgery, we offered him a complimentary LipiFlow treatment for the surgical eye.
It is not unusual for it to take time for patients to appreciate the change after thermal pulsation therapy. This patient, however, had an almost immediate improvement in symptoms. When I saw him two weeks after the treatment, he looked me in the eyes and said, “This has been life changing!”
He was much more comfortable and less light sensitive. His refraction was plano sphere, acuity had improved to 20/25+, and near vision had improved from 20/80 to 20/40. We decided to treat the second eye proactively and proceed with scheduling surgery for the left eye, which has since been delayed due to the coronavirus pandemic.
It is not clear whether this patient had undertreated MGD before surgery or whether it dramatically worsened due to the surgical insult and effect of topical drops. In any case, we were lucky that he ended up with a plano visual result and that the poor tear film quality didn’t affect the accuracy of IOL power calculations.
Ocular surface disease can lead to variability in keratometry and corneal astigmatism.4 MGD, in particular, can produce significant changes in the magnitude and axis of astigmatism, leading to changes in surgical treatment plans after thermal pulsation therapy.5 And even when the power is correct, the performance of multifocal IOLs suffers greatly in the presence of ocular surface disease. Thermal pulsation therapy helped this patient achieve what he wanted from a trifocal IOL in the first place and turned around his impressions of cataract surgery in our practice.
Case 3
A chatty 73-year-old European immigrant patient came to see us. She had 2+ nuclear sclerotic cataracts and chose to have femtosecond laser-assisted cataract surgery with a monofocal IOL. However, immediately following surgery on the first eye, the patient claimed that surgery had “ruined her vision.”
The surgery had been uneventful, and her refractive outcome was excellent with 20/20 visual acuity. At night, however, the patient was experiencing significant halo and glare, which she described as “Ferris wheels everywhere I look.” Although multifocal IOLs have a reputation for causing glare and halo, it is important to remember that these symptoms are also associated with ocular surface disease and can be disabling even in patients with monofocal IOLs.
We were somewhat mystified by the severity of the symptoms in this case, however, given the paucity of objective signs. We tried multiple approaches over the course of several months, including a scleral lens and aggressive dry eye therapy.
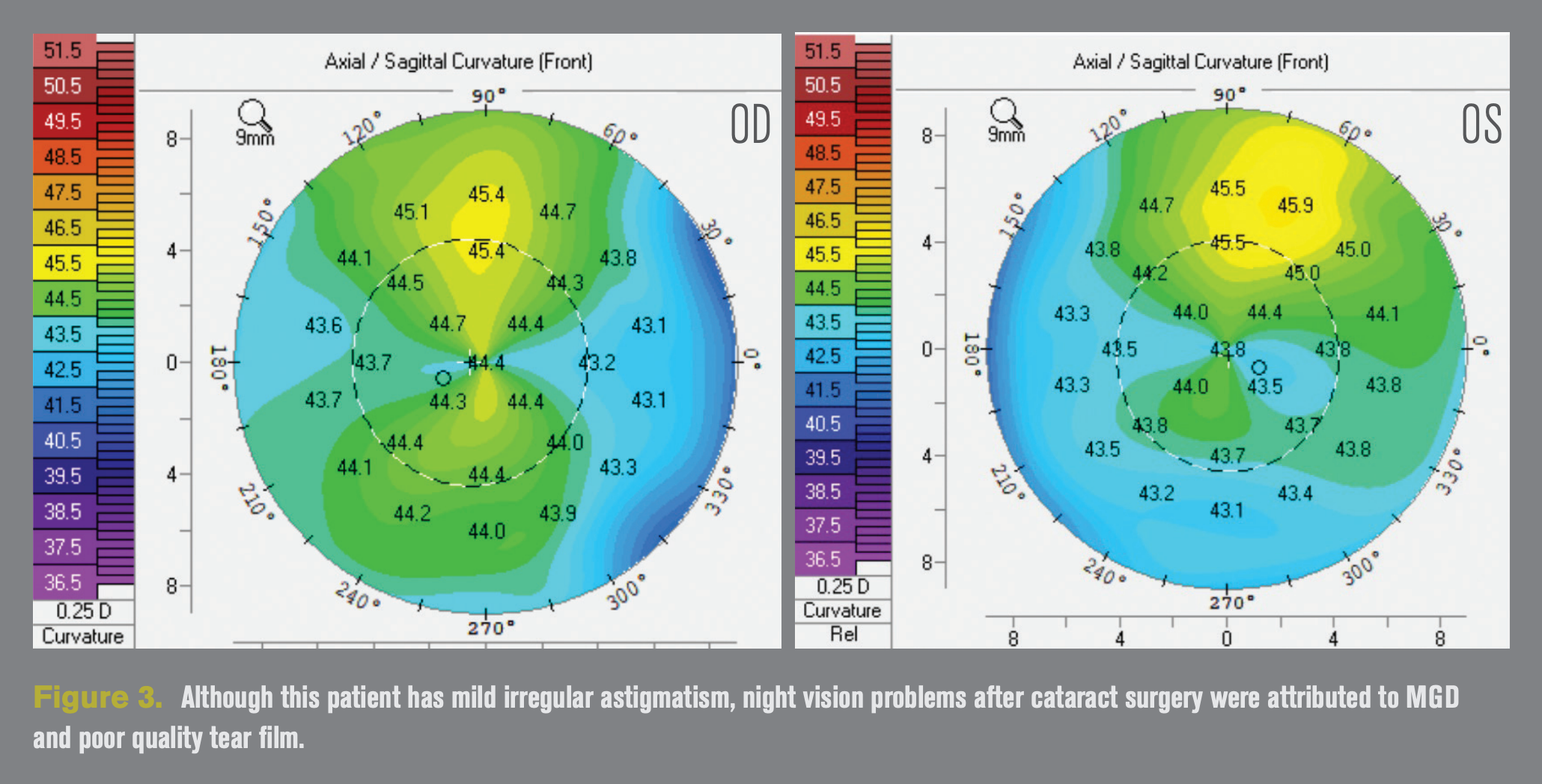
She had mild irregular astigmatism (Figure 3) and we wondered if this had been induced or worsened and was somehow responsible for her symptoms, although her topographies had not changed. However, nothing resolved or even improved the symptoms.
Finally, I convinced her to try thermal pulsation therapy. She was hesitant because neither hot compresses nor any amount of dry eye therapy had improved the glare. The results were tremendous. Her night vision symptoms were greatly reduced and she is now happier with her vision. This also clarified for her that the tear film, rather than the lens the surgeon had implanted, was responsible for her problems, overcoming her reluctance to have surgery on the second eye.
Had thermal pulsation taken place preoperatively for this patient, she may have still had symptoms, but they likely would have been minimized and perhaps the extensive chair time and hand-holding that was necessary to make this patient happy could have been avoided.
Conclusion
Management of the ocular surface can help to maximize surgical healing and recovery, improve comfort, and help patients achieve and maintain high quality vision after surgery. As these cases illustrate, it is far better to treat the ocular surface and meibomian glands before surgery than it is to deal with problems afterward.
References
1. Trattler WB, Majmudar PA, Donnenfeld ED, McDonald MB, Stonecipher KG, Goldberg DF. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017 Aug 7;11:1423-1430.
2. Alghamdi YA, Mercado C, McClellan AL, Batawi H, Karp CL, Galor A. Epidemiology of meibomian gland dysfunction in an elderly population. Cornea. 2016 Jun;35(6):731-5.
3. Cochener B, Cassan A, Omiel L. Prevalence of meibomian gland dysfunction at the time of cataract surgery. J Cataract Refract Surg. 2018 Feb;44(2):144-148.
4. Epitropoulos AT, Matossian C, Berdy GJ, Malhotra RP, Potvin R. Effect of tear osmolarity on repeatability of keratometry for cataract surgery planning. J Cataract Refract Surg. 2015 Aug;41(8):1672-7.
5. Matossian C. Impact of Thermal Pulsation Treatment on Astigmatism Management and Outcomes in Meibomian Gland Dysfunction Patients Undergoing Cataract Surgery. Clin Ophthalmol. 2020;14:2283-2289.
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.