Give toric ortho-k lenses a try
Patients with astigmatism can benefit from myopia management treatment
Myopia management is growing rapidly in popularity among the optometric community as well as with patients. Whether fitting a soft multifocal lens, figuring out when and how to prescribe atropine, or gaining confidence and success with orthokeratology (ortho-k) lenses, the quest for learning excites me.
In my 15 years as a progressive myopia manager, I have seen multiple changes in treatment strategies in the battle against progressive myopia. As technology improves, ODs can more easily advance treatments to a wider range of patients.
Astigmatism
One area of hesitation I see from colleagues is the treatment of myopic children who also have corneal astigmatism. Approximately 33.6% of Asian children have astigmatism,1 and in the United States astigmatism is–2.00 D or higher in 20% of children. Although soft toric multifocals and atropine are available for patients with astigmatism, many practitioners will choose ortho-k as a treatment option.2
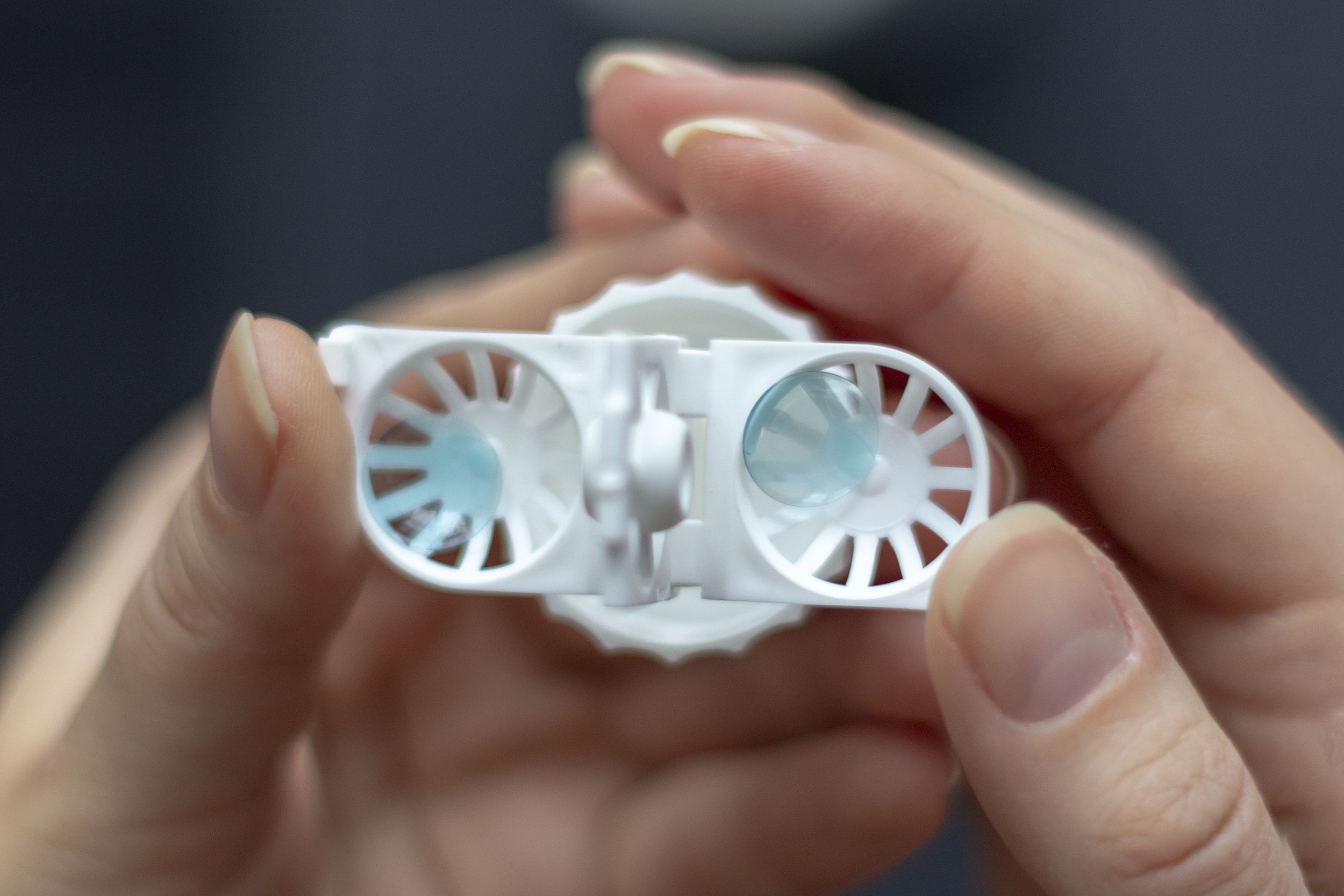
For a some of these patients, practitioners may find that spherical design lenses yield unsatisfactory results. As such, I have seen patients with astigmatism overlooked as potential candidates for ortho-k as a method for managing their myopia. This does not have to be the case. Understanding corneal elevation changes and how they affect centration and ultimately design choice can yield a rewarding addition to a myopia management practice.
Good centration
As clinicians, ODs have been trained to focus their efforts on the refractive error of their patients. Similarly, many ODs have focused only on the myopic correction component of FDA-approved ortho-k designs from –5.00 D to –6.00 D. I have seen multiple patients with corneal astigmatism passed over for treatment with ortho-k who could have been highly successful. However, for good centration and effective corneal molding on these asymmetrical corneas exhibiting elevation changes (toricity), understanding available toric designs is key to proper fit and treatment success.
ODs are familiar with the classic “bow tie” pattern of with-the-rule astigmatism when evaluating corneal topography maps. In the case of ortho-k, the size of the bow tie can be as important as the amount of astigmatism. When the bow tie is large and extends across the whole meridian of the topography, or the whole cornea, it is known as limbus-to-limbus astigmatism. Conversely, the bow tie may be small and contained within the central part (greater than 7 mm) of the cornea, and the peripheral cornea retains its more spherical shape. This is known as apical astigmatism.
The distinction between limbus-to-limbus corneal astigmatism and apical corneal astigmatism is critical for ortho-k success. Patients with apical astigmatism can often be fit with spherical or standard designs, such as Euclid Emerald, which will fit correctly along the periphery of the cornea and produce the 360˚ “sealed” ring pattern topography of a reverse geometry ortho-k lens design. This consistent ring is needed for the patient to achieve good myopia reduction. When a patient has limbus-to-limbus astigmatism, a considerable elevation difference exists between the steep (deep) and flat (shallow) meridians. Therefore, a spherical design lens will fit differently on these elevations even if the amount of refractive cylinder is the same.
On-eye lens decentration and poor visual results will be observed if the ring area lifts away from the primary meridians, especially if the superior and inferior areas are the same. In these cases, an asymmetrical toric design is needed to achieve the best centration and consistent myopia reduction.
The best way to look at pretreatment corneal astigmatism is with a topographer, using the apical or elevation map setting. This setting allows the user to scroll the cursor over the corneal map and measure the highest and lowest elevation readings compared with the baseline. Most of today’s topographers offer an elevation evaluation function, but users may need to contact their individual instrument’s guide to see exactly how to perform this function on a specific machine.
Practitioners may have various starting points for the amount of elevation difference that determines the chosen toric design. Clinically, I have determined that when the elevation difference is less than 25 μm between the primary meridians, I start with a standard spherical design. If the difference is greater than 25 μm or I see decentration with a spherical fit, then I will consider using a toric design. If the amount of corneal elevation is greater than 50 μm, I will begin with an empirically ordered toric design to align correctly on this patient’s cornea.
When a correctly designed ortho-k lens is worn overnight, the topography should show mid-peripheral alignment. This provides stabilization of the lens on the eye and creates the ideal hydrodynamic force under the lens to gently move the epithelial tissue into position for optimized ortho-k effects. The positive “push” or downward force of the tears behind the center of the lens (treatment zone) combines with the negative “upward pull” along the mid-peripheral areas of the cornea to create the ortho-k myopia reduction effects. If a patient has a large elevation difference between the meridians, they may have insufficient sealing of the fluid force area with resulting decentration and poor ring formation. For this reason the patient with limbus-to-limbus astigmatism requires a toric periphery design to align the fluid forces correctly in each meridian.
Toric designs have been shown to work. In 1 study looking at patients aged 9 to 16 years, the children wearing the toric design showed a 92.8% success rate.3 I have seen excellent results in my practice with improved centration and visual performance for patients who initially were fit in a spherical design and then switched into a toric design.
The process
The following are steps taken in the clinic for ortho-k patients:
– Screen all patients with a cycloplegic refraction, a short binocular vision assessment, and baseline axial topography.
– Discuss with parent and patient what clinical
findings have revealed and which treatment options are available to them. When clinically relevant, we make a strong recommendation for ortho-k. If the patient has corneal astigmatism, we discuss that specific finding and how successful they can be when we choose the correct lens design.
– When all questions are answered, evaluate the overall plan and achieve agreement and understanding of the process of return visits from the child and the parents.
– Gather all topographical elevation data and work directly with the contact lens laboratory consultants to place an order for the patient-specific design, shape, amount of lens toricity, and myopic correction target. One important learning is to underestimate the amount of lens toricity because too much will result in a tightly fitting lens and irregular visual results or superficial corneal staining.
– When the lens order arrives, application and removal training is scheduled. At that visit, we review with the patient the steps to proper cleaning, disinfecting, and storage of ortho-k lenses. We stress careful handling and teach them how to properly rub the lens in their palm and pick up a lens that has dropped posterior surface down on a table or counter. The next visit is scheduled for the following day or in several days, depending on patient specifics.
– At the first follow-up visit, we answer questions that arose during the patient’s first night of lens wear and determine if they followed the proper care steps. At this early stage, the topography tangential view will show the best evaluation of the treatment and rings beginning to form on the cornea. They may not be complete yet, but it is possible to evaluate general overnight positioning and the early ring formation for breaks. Another option is use of sodium fluorescein and the lens on eye to evaluate fit and ring formation for additional information to share with the lab consultant to make design changes. Remember that corneal tissue change speed is patient specific, so avoid quick changes. I usually hold changes until the 2-week follow-up visit, if possible.
Summary
Patients with corneal astigmatism should be offered the same opportunities for myopia management as their spherical counterparts. These patients are capable of similar ortho-k success. Consider evaluating patients for topographical elevation differences and choosing the appropriate toric designs. Toric ortho-k designs work. Consider giving them a try.
REFERENCES
1. Kleinstein RN, Jones LA, Hullett S, et al; Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error Study Group. Refractive error and ethnicity in children. Arch Ophthalmol. 2003;121(8):1141-1147. doi:10.1001/archopht.121.8.1141
2. Harvey EM, Dobson V, Clifford-Donaldson CE, Green TK, Messer DH, Miller JM. Prevalence of astigmatism in Native American infants and children. Optom Vis Sci. 2010;87(6):400- 405. doi:10.1097/OPX.0b013e3181d95b23
3. Fadel D. Reshaping ortho-k. Review Cornea Contact Lens. 2017:26-28. Accessed July 1, 2021. https://www. reviewofcontactlenses.com/CMSDocuments/2017/2/rcl0217i.pdf
Newsletter
Want more insights like this? Subscribe to Optometry Times and get clinical pearls and practice tips delivered straight to your inbox.